GENERAL MEDICINE ASSIGNMENT- MAY 2021
SOWJANYA REDDY PALAKURTHY
130
8th SEMESTER
I have been given the following cases to solve in an attempt to understand the topic of 'PATIENT CLINICAL DATA ANALYSIS' to develop my competency in reading and comprehending Clinical Data including History, clinical findings, Investigations, and diagnosis and come up with a treatment plan.
The Link to the questions asked : http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
The following are my answers to the Medical Assignment based on my comprehension of cases.
1. PULMONOLOGY
CASE-A
"A 55 Year Old Female with Shortness Of Breath, Pedal Edema and Facial Puffiness"
https://soumyanadella128eloggm.blogspot.com/2021/05/a-55-year-old-female-with-shortness-of.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: By observing the recent issues, the evolution of symptomatology in the patient would be the following:
- 1st The patient developed Grade 4 SOB due to the underlying lung pathology (COPD and Bronchiectasis).
- The disease then progressed causing Right heart failure, causing an increase in back pressure and decreased venous return → which caused Ankle Edema and Facial Puffiness.
- Due to decreased Venous return → decreased cardiac output → Left Heart failure → aggravated her SOB.
- Patient must've have developed renal failure as the rft was abnormal and it might have lead to facial puffiness, hypochloremia and hyponatremia.
- As more fluid is trapped in her extravascular space, there might be decreased urine output due to ADH release.
- Primary etiology is most probably her lungs( Bronchioles), due to dust exposure in paddy fields.
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: The pharmacological and non-pharmacological interventions used and their respective mechanisms are:
- Head And Elevation- It shows an improvement in transthoracic pressure.
- O2 - to maintain SPO2
- BiPAP - to deliver O2
- Amoxiclavulunate- Antibiotic (MOA- Beta- Lactam antibiotics inhibit Cell wall synthesis in susceptible bacteria)
- Azithromycin - To resolve infection(MOA - Bind to 50s Ribosomal subunit and inhibit protein synthesis)
- Inj. Lasix- Used as a diuretic for Hypertension(MOA- Loop diuretic- Increases the excretion of Na+ & water by the kidneys by inhibiting their reabsorption from PCT &DCT)
- Inj. Hydrocortisone - To treat Bronchiectasis(MOA- Glucocorticoid→ reduces inflammation by inhibiting Phospholipase A2)
- Tab. Pantop - Prevents acid secretion(MOA- PPI→ Inhibits final step of gastric acid production, in the gastric parietal cell, it binds to H+/K+/ATP Pump to inhibit gastric acid)
- Neb. with Ipravent, budecort - Anticholinergic bronchodilators( MOA- Relaxes Air passages)
- Ipratropium Bromide - Dilatation of air passages and to increase air flow(MOA- Acetylcholine Antagonist→ Decreases the production of cGMP By blocking Muscarinic cholinergic receptors )
- Tab. Pulmoclear - To relieve mucus (MOA - Bronchodilator & Mucolytic)
- Chest Physiotherapy - Used as an exercise for lungs and to wash out accumulated CO2
- I/O Charting - Input output charting is important
- Inj. Thiamine - It increases the oxygen concentration.(MOA- It combines with ATP in the Liver, kidneys, leukocytes → produces thiamine diphosphate→ acts as coenzyme in carbohydrate metabolism, trans-ketolation reactions and in utilization of hexose in hexose-monophosphate shunt)
- Temp, BP, PR, SPO2 Monitoring - Vitals
Q3: What could be the causes for her current acute exacerbation?
ANS: The exacerbation maybe due to presence of Heart failure along with kidney failure
Q4: Could the ATT have affected her symptoms? If so how?
ANS: Could have affected, because Isoniazid and rifampicin are nephrotoxic..
Q5: What could be the causes for her electrolyte imbalance?
ANS: The electrolyte imbalances are due to heart and renal failure.
2. NEUROLOGY
CASE-A
"A 40 Year Old Male with Irrelevant Talking and decreased Food Intake"
https://143vibhahegde.blogspot.com/2021/05/wernickes-encephalopathy.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: The patient is a chronic alcoholic, which proves a very important risk factor in his condition.
- Alcohol is a CNS depressant that produces altered behavior.
- Due to prolonged usage alcohol causes increased physical and psychological dependance.
- 2 Years ago - The patient was diagnosed with DM
- 1 Year ago - The patient had a seizure
- 4 Months ago - He again had a seizure due to cessation of alcohol
- 10 Days ago - He had genralized Body pains
- 9 Days ago - Patient started talking to himself, laughing( altered behavior), unable to lift himself off the bed and move around, decreased food intake. Because he stopped drinking.
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: The pharmacological and non-pharmacological interventions used in this patient are:
- IVF NS and RL - To treat dehydration
- Inj. Thiamine - To treat vitamin B1 deficiency in chronic alcoholics(MOA- It combines with ATP in the Liver, kidneys, leukocytes → produces thiamine diphosphate→ acts as coenzyme in carbohydrate metabolism, trans-ketolation reactions and in utilization of hexose in hexose-monophosphate shunt)
- Inj. Lorezepam - It treats seizures( MOA- It binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated Cl Channel→ it enhances inhibitory effect of GABA, Which enhances the conductance of Cl ions into the call )
- Tab. Pregabalin - It also reduces seizures and excitability( MOA- Inhibition of Alpha 2 delta subunit of voltage-gated Cl channels)
- Inj. HAI SC- to treat Diabetes(MOA- Short Acting Insulin )
- GRBS - General Random Blood Sugar Monitoring
- Lactulose - To relieve constipation, if any( MOA- Laxative )
- Inj. KCl - Used to treat hypokalemia
- Syp. Potchlor - To prevent and treat low levels of potassium in the body(MOA- Restores normal levels of K)
Q3: Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
ANS: Chronic long term addiction may impose effect on neurological system, liver, pancreas and even effects the normal homeostasis of the body by altering various nutrient levels.
* The alteration in the various nutrients, vitamins and mineral levels might have caused the occurrence of neurological symptoms.
Q4: What is the reason for giving thiamine in this patient?
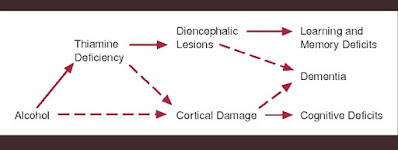
ANS: It is very important to administer thiamine in an Alcoholic because they are at severe risk of being deficient, and it may lead to the development of Wernicke's Korsakoff Syndrome, Cerebellar degeneration, and cardiovascular dysfunction.
Q5: What is the probable reason for kidney injury in this patient?
ANS: The sudden alcohol withdraw might be the probable cause for kidney failure.
Q6: What is the probable cause for the normocytic anemia?
ANS: The normocytic anemia is due to kidney failure.
Q7: Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
ANS: Yes, chronic alcoholism may have aggravated foot ulcer formation.
* Excessive alcohol abuse leads to decrease in nutrients→ if tissue or nerve injury occurs →it delays or effects the healing process→ leads to ulcer formation.
CASE-B
"A 52 Year Old Male with Cerebellar Ataxia"
https://kausalyavarma.blogspot.com/2021/05/a-52-year-old-male-with-cerebellar.html?m=1
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: Giddiness →This was associated with vomiting on the same day.
- After 3 days he consumed a small amount of alcohol, developed giddiness getting up from the bed and while walking.
- This was associated with Bilateral Hearing loss, aural fullness and presence of tinnitus.
- He has associated vomiting.
- The anatomical localization in most probably the Cerebral Blood vessels
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
- MVT methylcobalamin - for B12 deficiency
- Tab. Vertin - To treat inner ear problems (MOA- Betahistine improves the microcirculation in the ear. It is an agonist of H1 Receptors and antagonist of H3 Receptors)
- Inj. Zofer - Antiemetic medication (MOA - It binds to the receptor 5-HT3 →Inhibits the binding of serotonin→ prevents nausea and vomiting)
- Tab. Ecosprin - Anti- platelet medication (MOA- Inhibits the formation of Thromboxane A2, By blocking Cyclooxygenase)
- Tab. Atorvostatin - It is a statin used to decrease cholesterol levels (MOA- Inhibits HMG-CoA Reductase)
- Tab. Clopidogrel - as an anti platelet medication, used to prevent blood clots.( MOA- It selectively inhibits the binding of ADP to its Platelet P2Y12 Receptor→ ADP Mediated activation of Glycoprotein GPIIb/IIIa complex → Inhibits platelet aggregation which is irreversible )
- Inj. Thiamine - to treat for B1 deficiency(MOA- It combines with ATP in the Liver, kidneys, leukocytes → produces thiamine diphosphate→ acts as coenzyme in carbohydrate metabolism, trans-ketolation reactions and in utilization of hexose in hexose-monophosphate shunt)
ANS: *Might have contributed as the patient didn’t use medication and it is a risk factor for stroke.
Q4: Does the patients history of alcoholism make him more susceptible to ischemic or hemorrhagic type of stroke?
ANS: Yes it makes him susceptible for both hemorrhagic and ischemic stroke as he seems to be a chronic alcoholic and consumes more alcohol.
CASE-C
"A 45 Year Old Female with Palpitations, Pedal edema, Chest Pain, Chest Heaviness, Radiating pain along Left Upper Limb"
http://bejugamomnivasguptha.blogspot.com/2021/05/a-45-years-old-female-patient-with.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: The evolution of symptoms are as follows:
- 8 months ago - Developed EDEMA in both the legs
- 6 days ago - developed pain along her left upper limb associated with tingling and numbness
- 5 days ago - Chest pain and breathlessness, and increased heart rate.
- The anatomical localization of this etiology is the cervical spine.
- Primary etiology is due to hypokalemia
Q2: What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
ANS: Hypokalemic periodic paralysis, risk factor is the usage of diuretics.
Q3: What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ANS: The ECG changes seen in hypokalemia are:
- T Wave - Flattening and Inversion (mild cases)
- Q-T Interval - Prolongation
- U Wave - Visible
- ST - Depression (Severe cases)
CASE-D
"A 55 Year Old Male with Seizures"
https://rishikoundinya.blogspot.com/2021/05/55years-old-patient-with-seizures.html
QUESTION AND ANSWERS
Q1: Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
ANS: Yes, there is a relation between Stroke and seizures.
- In this patient stroke causes ischemia and infraction which may cause loss of brain parenchyma which is followed by a gliosis as a result late response.
- Epileptic foci resulting from brain injury are characterized by areas of intense fibrillary gliosis bordering neuronal tissue.
- The known pathological changes that occur in gliosis may impair glial control of extracellular potassium ions and lead to excessively excitable neuronal border regions.
- It also decreases the seizure threshold.
- Seizures also increase the chances of having a recurrent infract which may lead to more brain tissue involvement.
- An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarization, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypo-perfusion, and hyper-perfusion injury (particularly after carotid end arterectomy) is an acute onset seizures pathology.
Q2: In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
ANS: *Initially patient had a Focal seizures without loss of consciousness(simple partial seizures) which usually follow after trauma or stroke
*In this patient due to temporal lobe involvement and gliosis it might have progressed to complex partial seizures or GTCS with more brain parenchyma involvement
CASE-E
"A 48 Year Old with Seizures and Altered Sensorium"
https://nikhilasampathkumar.blogspot.com/2021/05/a-48-year-old-male-with-seizures-and.html?m=1
QUESTION AND ANSWERS
Q1: What could have been the reason for this patient to develop ataxia in the past 1 year?
ANS: Alcohol-related ataxia→ the symptoms affect gait (walking) and lower limbs more than arms and speech. It can also cause associated signs of peripheral neuropathy.
*It may be due to injury to cerebellum or cerebrum due to intoxication and could also be due to thiamine deficiency.
*And frequent falls which are not attended by patients must have added to the effect.
Q2: What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses?
ANS: Chronic heavy and binge ethanol consumption is likely linked to the occurrence and clinical worse outcome of ICH and frequent falls might have aggravated.
CASE-F
"A 30 Year Old with Weakness of Right Upper Limb and Lower Limb"
QUESTION AND ANSWERS
Q1: Does the patient's history of road traffic accident have any role in his present condition?
ANS: Yes, the history of road traffic accidents might have played an important role in his current condition by the following means:
- WHIPLASH- It may cause damage to the Carotid Artery
- Disruption of Blood supply - to the Brain
- Brain Hemorrhage ( brain Bleed)
Q2: What are warning signs of CVA?
ANS: The warning signs of CVA are:
- Sudden NUMBNESS or WEAKNESS in the face, arm, or leg especially on one side of the body.
- Sudden CONFUSION, trouble speaking, or difficulty understanding speech.
- Sudden TROUBLE WALKING, dizziness, loss of balance, or lack of coordination.
- Sudden SEVERE HEADACHE with no known cause.
Q3: What is the drug rationale in CVA?
ANS: The drugs used are:
- Inj. Mannitol - Decreases the cerebral edema (MOA- Osmotic effect)
- Tab. Ecosprin - Anti- Platelet effect (MOA- Inhibits the formation of Thromboxane A2, By blocking Cyclooxygenase)
- Tab. Atorvas - It decreases the cholesterol levels (MOA- Inhibits HMG-CoA Reductase)
Q4:Does alcohol has any role in his attack?
ANS: No, The patient consumes alcohol only occasionally, so it doesn't have any major role.
Q5: Does his lipid profile has any role for his attack?
ANS: The HDL levels, are way lower than the normal range.
* Low HDL is a known risk factor for stroke as it is a GOOD CHOLESTEROL.
CASE-G
"A 50 Year Old with Cervical Myelopathy"
https://amishajaiswal03eloggm.blogspot.com/2021/05/a-50-year-old-patient-with-cervical.html
QUESTION AND ANSWERS
Q1: What is myelopathy hand ?
ANS: A characteristic dysfunction of the hand, it is seen in various Spinal disorders where there is an involvement of the Spinal cord.
It occurs mainly due to PYRAMIDAL TRACT INVOLVEMENT.
*It is loss of power of ADDUCTION and EXTENSION Of the two or three Ulnar fingers.
*There is inability to hold(grip) and release rapidly with this fingers.
* Diagnosis is made by two important tests → Finger Escape Sign & Inability to grip and release
Q2: What is finger escape Sign?
ANS: It is the deficient adduction or extension of the ulnar two or three fingers.
*Also called: WARTENBERG'S Sign.
*Patient holds fingers extended and adducted for 30 seconds. Positive finding is abduction and flexion of ulnar two or three digits.
*Grading of Finger Escape Sign:
Q3: What is Hoffman's Reflex?ANS: It is an Involuntary Flexion movement of the thumb or index finger when the examiner flicks the fingernail of the middle finger down.
*The reflexive pathway causes a thumb to flex and adduct quickly.
* Absence indicates Inflammatory demyelinating polyneuropathy.
CASE-H
"A 17 Year Old with Seizures"
https://neerajareddysingur.blogspot.com/2021/05/general-medicine-case-discussion.html?m=1
QUESTION AND ANSWERS
Q1: What can be the cause of her condition ?
ANS: Her condition may be due to Iron Deficiency Anemia.
Q2: What are the risk factors for cortical vein thrombosis?
Q3:There was seizure free period in between but again sudden episode of GTCS why ?resolved spontaneously . why?
ANS: There was presence of seizure free period due to administration of antiepileptic drugs, as the effect wears off , the seizures re-appear.
Q4: What drug was used in suspicion of cortical venous sinus thrombosis?
ANS: CLEXANE
3.CARDIOLOGY
CASE-A
"A 78 Year Old Male with Shortness Of Breath, Chest Pain, B/L Pedal Edema and Facial Puffiness"
https://muskaangoyal.blogspot.com/2021/05/a-78year-old-male-with-shortness-of.html
QUESTION AND ANSWERS
Q1) What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
ANS:
Q2:Why haven't we done pericardiocenetis in this patient?
ANS: The patient developed moderate pericardial effusion and is diagnosed with heart failure, it is contraindicated and moreover the effusion was self-healing. It is an invasive procedure and in this patient it could be managed by consevrative therapy .
Q3: What are the risk factors for development of heart failure in the patient?
ANS: Risk factors are -
- Alcohol consumption
- Smoking
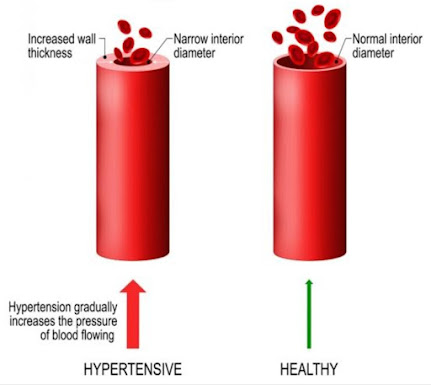
- Hypertension
Q4: What could be the cause for hypotension in this patient?
ANS: It is due to diastolic dysfunction.
CASE-B
"A 73 Year Old Male with Pedal Edema, Shortness Of Breath and Decreased Urine Output"
https://muskaangoyal.blogspot.com/2021/05/a-73-year-old-male-patient-with-pedal.html
QUESTION AND ANSWERS
Q1: What are the possible causes for heart failure in this patient?
ANS: The causes of heart failure can be:
- Hypertension
- Diabetes
Q2: what is the reason for anemia in this case?
ANS: Diabetes may cause kidney failure, which in-turn may pre-dispose to anemia.
Q3: What is the reason for blebs and non healing ulcer in the legs of this patient?
ANS: The patient is diabetic, so the healing process is pretty slow or impaired.
* Adequate amount of blood supply is required for adequate healing to occur, in this case it is insufficient
* Improper circulation, explains the blebs and non-healing ulcer in this patient.
Q4: What sequence of stages of diabetes has been noted in this patient?
ANS: Sequence of stages are:
- STAGE 1 - DM Type 2
- STAGE 2 - Insulin resistance
- STAGE 3 - diabetic retinopathy
- STAGE 4 - PVD
CASE-C
"A 52 Year Old Male with A-Fib and Bi-atrial Thrombus"
https://preityarlagadda.blogspot.com/2021/05/biatrial-thrombus-in-52yr-old-male.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: The anatomical site is Blood vessels
* The evolution of symptoms are:
- 10 Years ago- The patient underwent a surgery for Inguinal Hernia
- 3 Years ago - The Patient did an NSAID abuse and facial puffiness was also present.
- 2 Years ago - Facial puffiness was present
- 1 Year ago - SOB Grade II And HTN
- 2 days ago- The patient complained of constipation and decreased urine output, SOB Grade II which progressed to Grade IV
- Present day morning- Showcased Anuria
- The primary etiology is mainly Hypertension aggravated ATHEROSCLEROSIS
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: The pharmacological and non-pharmacological interventions used are:
- Tab. Dytor - Reduces Edema (MOA- Diuretic - Increases the amount of urine excretion, thus relieving SOB and swelling in arms, legs and abdomen)
- Tab. Acitrom (MOA- Inhibits the action of Vitamin K-epoxide reductase, which is required for regeneration &maintaining levels of vitamin K reuired for blood clotting )
- Tab. Cardivas - Alpha and Beta blocker (MOA- Carvedilol blocks epinephrine , which inversely lowers your heart rate)
- Inj. HAI SC - To treat diabetes(MOA- Short Acting Insulin )
- Tab. Digoxin - Used to treat arrhythmias ( MOA- Inhibits the activity of myocardial Na-K ATPase pump)
Q3: What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
ANS: The Pathophysiology of Cardio-Renal syndrome is as follows:
* In this patient it is TYPE- 4
Q4: What are the risk factors for atherosclerosis in this patient?
ANS: The major risk factor for atherosclerosis in this patient is HTN.
Q5: Why was the patient asked to get those APTT, INR tests for review?
ANS: APTT & INR tests are done frequently when a person is prescribed Anticoagulant drugs such as warfarin, to check if the Drug is producing the required, optimum function.
CASE-D
"A 67 Year Old with Acute Coronary Syndrome"
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: The evolution of symptoms is as follows:
- 12 Years ago - The patient was diagnosed of DM-Type 2
- 1 Year ago - He had heartburn
- 7 months ago - TB +ve
- 6 months ago - HTN
- 1/2 Hour ago - SOB
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: The pharmacological and non-pharmacological interventions used in this patient are:
- Met XL - Beta blocker long acting(MOA- It acts by inhibiting epinephrine)
- PCI - Percutaneous Coronary Intervention - Used to open blood vessels in heart that have been narrowed due to atherosclerosis (MOA- It is a non-surgical procedure that uses a catheter to place stents which open blood vessels blocked due to plaque)
Q3: What are the indications and contraindications for PCI?
ANS: INDICATIONS
- Acute ST-Elevation Myocardial Infarction (STEMI)
- Non-ST-Elevation Acute Coronary Syndrome(NSTE-ACS)
- Unstable and stable angina
- High risk test findings
- Coagulopathy
- Decompensated congestive heart failure
- Uncontrolled HTN
- Pregnancy
- Active Infection
- Renal Failure
Q4: What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on over testing and overtreatment important to current healthcare systems?
ANS: If PCI is done in patient who doesn't need it, it causes Increased, uncontrolled bleeding and stent thrombosis.
CASE-E
"A 60 Year Old with Acute Myocardial Infarction"
https://bhavaniv.blogspot.com/2021/05/case-discussion-on-myocardial-infarction.html?m=1
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: The evolution of symptoms is as follows:
- Firstly the patient developed Chest pain and was radiating to his back and then the patient developed giddiness.
- As the character of pain is Dragging and Radiating type and not burning, we can localise it to the heart.
- On further investigations, it was found to be INFERIOR WALL MYOCARDIAL INFARCTION.
- The known sequelae might be: Patient is diabetic + hypertensive →Endothelial Injury→ leads to Thrombus formation and occlusion→ MI.
- The site of anatomical localization is blood vessels
Q2: What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: The Pharmacological and Non-pharmacological interventions used in this patient are:
- Asprin - Analgesic and antiplatelet effect (MOA- Inhibits COX activity)
- Atorvastatin- Used to decrease the cholesterol levels - It is a statin used to decrease cholesterol levels (MOA- Inhibits HMG-CoA Reductase)
- Clopidogrel - Anti-platelet effect and prevents further aggregation( MOA- It selectively inhibits the binding of ADP to its Platelet P2Y12 Receptor→ ADP Mediated activation of Glycoprotein GPIIb/IIIa complex → Inhibits platelet aggregation which is irreversible )
- Insulin - Hypoglycemic effect and used as an emergency intervention in this patient.
- Angioplasty- Used to widen obstructed vessels
Q3: Did the secondary PTCA do any good to the patient or was it unnecessary?
ANS: It was not necessary. It was not a better option in this patient because it was done after 3 days of the symptoms onset and stent has its own complications of re-thrombosis. Ideally it should be done before 12 hrs of onset of symptoms.
4.GASTROENTEROLOGY
CASE-A
"A 33 Year Old with Pancreatitis, Pseudocyst and Left Broncho-Pleural Fistula"
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-pancreatitis-with.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: *The evolution of symptoms in the patient are as follows:
- 5 Years ago - Abdominal pain and vomiting
- 3 Years ago - Recurrent episodes of pain and vomiting
- 20 days ago - Increased alcohol consumption
- 1 Week ago - Abdominal pain and vomiting due to excessive alcohol consumption
- 4 Days ago - Fever , constipation and burning micturition,
Q2: What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS: The pharmacological and non-pharmacological interventions used in this patient are:
- Meropenam - Antibiotic ( MOA- It inhibits cell wall synthesis similarly like beta lactam antibiotics)
- Metrogyl - Metronidazole (MOA- Enters organism→ interacts with DNA→ Disrupts the helical structure of DNA→ Causes DNA breakage→ Inhibits protein synthesis)
- Amikacin - used to treat bacterial infections ( MOA- Aminoglycoside - It binds to bacterial 30s ribosomal subunits and interferes with mRNA Binding and tRNA Acceptor sites, interfering with bacterial growth )
- Octreotide - decreases the release of growth stimulating hormones( MOA - It suppresses Insulin secretion)
- Pantop -Prevents acid secretion(MOA- PPI→ Inhibits final step of gastric acid production, in the gastric parietal cell, it binds to H+/K+/ATP Pump to inhibit gastric acid)
- Thiamine - It increases the oxygen concentration.(MOA- It combines with ATP in the Liver, kidneys, leukocytes → produces thiamine diphosphate→ acts as coenzyme in carbohydrate metabolism, trans-ketolation reactions and in utilization of hexose in hexose-monophosphate shunt)
- Tramadol - Analgesic ( MOA - It is a Mu opioid receptor agonist and SNRI)
CASE-B
"A 25 Year Old Male with Epigastric Pain"
https://nehae-logs.blogspot.com/2021/05/case-discussion-on-25-year-old-male.html
QUESTION AND ANSWERS
Q1: What is causing the patient's dyspnea? How is it related to pancreatitis?
ANS: Pleural Effusion might be causing the patient's dyspnea
* Presence of pleural effusion is currently considered an indication of severe pancreatitis and not merely a marker of the disease.
Q2: Name possible reasons why the patient has developed a state of hyperglycemia.
ANS: The patient has developed hyperglycemia due to following cause:
- Destruction of Beta cells causes decrease synthesis and production of insulin
Q3: What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
ANS: The LFT's are elevated due to HEPATOCYTE INJURY.
* An AST to ALT ratio of over 2 is highly suggestive of Alcoholic liver disease.
Q4:What is the line of treatment in this patient?
ANS: INVESTIGATIONS
- 24 Hour urinary protein
- Fasting and Post prandial blood glucose
- HbA1c
- USG Guided pleural tapping
- IVF: 125ml/hr
- Inj. PAN 40mg IV OD
- Inj. ZOFER 4mg IV sos
- Inj. TRAMADOL 1 amp in 100ml NS, IV sos
- Tab. DOLO 650mg sos
- GRBS Charting 6th hourly
- BP Charting 8th hourly
"A 45 Year Old Female with Fever, Pain Abdomen, Decreased Urine Output and Abdominal Distension"
https://chennabhavana.blogspot.com/2021/05/general-medicine-case-discussion-1.html
QUESTION AND ANSWERS
Q1: what is the most probable diagnosis in this patient?
ANS: Ruptured liver abscess, Haemoperitonium
Q2: What was the cause of her death?
ANS: Shock due to excessive blood loss
Q3: Does her NSAID abuse have something to do with her condition? How?
ANS: Yes, NSAID induced hepatitis
5.NEPHROLOGY & UROLOGY
CASE-A
"A 52 Year Old , Post TURP with Non-Oliguria ATN Diabetic Nephropathy'
https://kavyasamudrala.blogspot.com/2021/05/medicine-case-discussion-this-is-online.html
QUESTION AND ANSWERS
Q1: What could be the reason for his SOB ?
ANS: It is a complication of TURP and also due to Metabolic acidosis
Q2: Why does he have intermittent episodes of drowsiness ?
ANS: Due to increased creatinine levels.
Q3: Why did he complaint of fleshy mass like passage in his urine?
ANS: It may be due to Urosepsis
CASE-B
"An 8 Year Old with frequent Urination"
https://drsaranyaroshni.blogspot.com/2021/05/an-eight-year-old-with-frequent.html
QUESTION AND ANSWERS
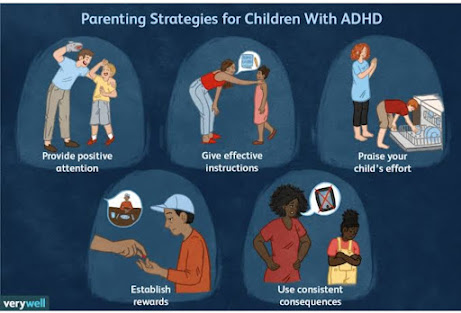
ANS: It is due to ADHD (Attention Deficit Hyperactivity Disorder)
Q2: How would you want to manage the patient to relieve him of his symptoms?
ANS: Medications such as Concerta , clonidine can be used
* Friendly school and home environments.
6. INFECTIOUS DISEASES (HIV-Virus, Mycobacteria, Gastroenterology,Pulmo)
CASE-A
"A 40 Year Old Female with Dysphagia, Fever and Cough"
https://vyshnavikonakalla.blogspot.com/2021/05/a-40-year-old-lady-with-dysphagia-fever.html
QUESTION AND ANSWERS
Q1: Which clinical history and physical findings are characteristic of tracheo-esophageal fistula?
ANS: History of coughing after taking food since 2 months, as the food through fistula had passed into trachea and stimulated the cough receptors.
*On barium swallow there is leakage of contrast into left bronchi.
Q2: What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANS: There is very less chance that patient might be developing immune reconstitution inflammatory syndrome as the CD4 counts were not very less during the start of treatment. *It Could be due to TB or any opportunistic infections or neoplasm.
7. INFECTIOUS DISEASE & HEPATOLOGY
CASE-A
"A 55 Year Old Male with Liver Abscess"
https://kavyasamudrala.blogspot.com/2021/05/liver-abscess.html
QUESTION AND ANSWERS
Q1: Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ? What could be the cause in this patient ?
ANS: Alcohol is an important risk factor for the formation of both amoebic and pyogenic liver abscess.
Q2: What is the pathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
ANS:
Q3: Is liver abscess more common in right lobe ?
ANS: Yes, Liver abscess( about 50%) occurs more in the right lobe of the liver.
*Because it is a significant part with more blood supply, less commonly in left liver lobe or caudate lobe.
Q4: What are the indications for ultrasound guided aspiration of liver abscess ?
ANS: Indications are
- Non- responsive cases to conservative therapy
- Septicemia
- Left lobe abscess not amenable to percutaneous drainage
- Haemorrhage with or without intraperitoneal rupture of abscess ( life-threatening)
CASE-B
"A 21 Year Old Male with Liver Abscess"
https://63konakanchihyndavi.blogspot.com/2021/05/case-discussion-on-liver-abcess.html
QUESTION AND ANSWERS
ANS: Entamoeba histolytica
Q2: How do you approach this patient ?
ANS:
ANS: To provide complete and apt treatment
ANS: Serological testing is used for confirmation of amoebic liver abscess
8. INFECTIOUS DISEASES(Mucormycosis, Ophthalmology,Otolarnyngology& Neurology)
CASE-A
"A 50 Year Old Male with Altered Sensorium"
http://manikaraovinay.blogspot.com/2021/05/50male-came-in-altered-sensorium.html
QUESTION AND ANSWERS
Q1: What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: Evolution of symptoms in this patient is:
- 3 Years ago - Diagnosed with HTN
- 18/04/2021 - Had COVID-19 Vaccination and developed fever with chills and rigors
- 21/04/2021 - Same complaints and not relieved by medication
- 28/04/2021 - Generalized weakness , facial puffiness and periorbital edema and drowsy
- 4/05/2021 - weakness of upper & lower limbs, periorbital edema and facial puffiness was present
Q2: What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS: Drugs used are:
- Inj. Amphotericin B - Antifungal agent (MOA - It binds with ergesterol, a component of fungal cell membranes, forming pores that cause rapid leakage of monovalent ions (K+, Na+, H+, Cl- and causes fungal death)
- Deoxycholate Amphotericin B - Antifungal agent
Q3: What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
ANS:
9. INFECTIOUS DISEASES(COVID-19)
CASE-1
" COVID-19 With Co-morbidity. ( Pulmonology/ Rheumatology)
https://nikhilasampathkumar.blogspot.com/2021/05/covid-pneumonia-in-pre-existing-case-of.html
QUESTION AND ANSWERS
Q1: How does the pre-existing ILD determine the prognosis of this patient?
ANS: Patients with ILD already have a poor lung reserve and reduced gaseous exchange and their oxygen saturation’s are less. They have less viable lung tissue. On top of that COVID caused lung endothelial damage and further decrease saturations. Patient may also develop pulmonary artery hypertension with chronic hypoxia. So patient may develop complications at a low threshold. Studies have shown that there’s high mortality in patients with ILD and severe COVID . As the patient seems to be moderately effected by COVID complications could be less. SARS-CoV-2 infects cells with ACE2 as a receptor, and the reduced infection rate of COVID-19 in patients with ILD has been proposed to be due to decreased angiotensin II mRNA activity in the lung in ILD. This same study stated that although the risk of infection might be lower in patients with ILD, once infected, the severity and prognosis are worse in patients with ILD due to aggravated inflammatory responses and coagulopathy.
ANS: Steroids given for COVID doesn’t effect rheumatoid arthritis as it one of the medication for rheumatoid arthritis. While it can precipitate hypothyroidism as steroids prevent the peripheral conversion of T4 T3 and also decreases TSH production. So hypothyroidism could be precipitated.
Q3: Would this patient have an increased risk for post COVID autoimmune response compared to patients without a history of autoimmune disease?
ANS: Given that there has been no increase in exacerbations of RA patients concomitantly suffering from COVID-19 and no increase in new cases during the pandemic so far. Theatrically it may be true but practical evidence is not yet established. SARS-CoV-2 may trigger autoimmunity phenomena associated with a state of transient immunodeficiency of components of both innate and acquired immunity in which the immune system fails to properly recognize of autoantigens. This is associated a form of immune reconstitution that would magnify this anomaly in the convalescence of the disease
Q4: Why was she prescribed clexane (enoxaparin)?
ANS: Acute inflammation promotes a hypercoagulable state that may increase the risk of deep vein thrombosis (DVT) and pulmonary embolism. In chronic inflammatory disease such as rheumatoid arthritis (RA), pro-coagulatory factors are up-regulated.
CASE-2
"COVID-19 With diabetes"
https://nehapradeep99.blogspot.com/2021/05/a-50-year-old-female-with-viral.html
QUESTION AND ANSWERS
Q1: Since patient didn't show any previous characteristic diabetes signs, did the Covid-19 infection aggravate any underlying condition and cause the indolent diabetes to express itself? If so what could be the biochemical pathways that make it plausible?
ANS: In human monocytes, elevated glucose levels directly increase SARS-CoV-2 replication, and glycolysis sustains SARS-CoV-2 replication via the production of mitochondrial reactive oxygen species and activation of hypoxia-inducible factor 1α. Therefore, hyperglycemia might support viral proliferation
This large burden of inflammatory cells can affect the functions of skeletal muscle and the liver, the major insulin-responsive organs that are responsible for the bulk of insulin-mediated glucose uptake. In addition, patients with severe COVID-19 show muscle weakness and elevation of liver enzyme activities, which might suggest multiple organ failure, particularly during a cytokine storm
In individuals with obesity, pro-inflammatory cytokines with a T helper type 1 cell signature are known to increase insulin resistance
The SARS-Cov-2 tropism for the β-cell could cause acute impairment of insulin secretion or destruction of β-cells resulting in de novo development of diabetes
Q2: Did the patient's diabetic condition influence the progression of pneumonia?
ANS: A. The airway surface liquid (ASL) plays a pivotal role in lung defense. Diabetes is related with higher ASL glucose concentration, ASL volume accumulation in alveolar space, imbalance of reactive oxidative species (ROS), and inflammatory chemokine production.
B. The COVID-19 infection promotes injuries in type I and type II pneumocytes and lung endothelial lesions, with subsequent additional secretion of protein-rich exudate in the alveolar space and intravascular coagulation in lung vessel, which leads to a reduction in surfactant and gas exchange.
C. The association between diabetes and SARS-CoV-2 increases the glucose and protein concentration in ASL, leading to increase the risk of pneumonia.
Bearing in mind the osmotic effect due to the high ASL glucose concentration, these changes could explain the higher total water content in lung during hyperglycemic condition, which can be related with higher volume of ASL, leading to reduced gas exchange rates of O2 and CO2 between alveolar space and lung capillaries. Frequently, the mild increase in ASL can be compensated by ventilatory response mechanisms. It is important to point out that the pathological reduction of O2 and CO2 exchange through the lumen of pneumocytes and blood occurs in poorly controlled diabetic patients mainly under bacterial, inflammatory, or oxidant disruptions.
The high concentration of glucose and the increased volume in the ASL are maintained mainly by the low expression of SGLT1 in the apical membrane of type I and II pneumocytes in the lungs of diabetics. Hyperglycemia promotes increased paracellular glucose transport from blood to ASL. The evolution of DM promotes activation of the inflammatory cascade with the production of interleukins, increased ROS, and endothelial damage. These changes provide an increased risk for pneumonia due to the proliferation of bacteria P. aeruginosa and MRSA.
Q3: What is the role of D Dimer in the monitoring of COVID? Does it change management or would it be considered over-testing?
ANS: Elevated baseline D-dimer levels are associated with inflammation but not with VTE score in COVID-19 patients, suggesting that it is unreasonable to judge whether anticoagulation is needed only according to D-dimer levels. However, the abnormal changes of D-dimer and inflammatory factors suggest that anticoagulant therapy might be needed.















Hi
ReplyDelete