CASE DISCUSSION ON YOUNG-ONSET HYPERTENSION
This is an online E-Log book to discuss our patient's de-identified data shared after taking his/her/Guardian's signed informed consent. Here, we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve these patient's clinical problems with collective current best evidence-based inputs. This E-log also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box are welcome.
HOPI: The patient was apparently asymptomatic 2 months ago and then developed headache which was not continuous (on and off). It was insidious in onset and progressive in nature, Headache was of throbbing type. He also complained of increase in frequency of attacks.
*The headache gets aggravated on increased work load and stress and decreased on taking rest /sleeping.
*On regular health checkup in their workplace he was diagnosed with Hypertension 1 year ago but did not take any medication for it as such.
*No H/O of Fever, Nausea, Blurring of vision, watering of eyes, SOB, Pedal Edema, chest discomfort, Facial puffiness or any weakness in body parts.
* He came to the OPD again on 3/05/2021 for follow-up
PAST HISTORY: No similar complaints in the past
*Patient is a K/C/O HTN since 1 year and is not on any medication.
* N/K/C/O: DM, TB, BA, Epilepsy
PERSONAL HISTORY:
- Diet - Mixed ( Salt intake- Normal)
- Appetite- Normal
- Sleep- Adequate , but sometimes disturbed due to stress and increased headache
- Bowel and Bladder movements- Regular
- No addictions
- No allergies
FAMILY HISTORY: The patient's father had HTN and died due to renal failure.
* No H/O DM
GENERAL EXAMINATION: The Patient was examined in a well lit room after taking informed consent.
He was Conscious, coherent, cooperative at the time of examination, Well oriented to time, place and person.
- The patient is well built and nourished
- Pallor: Absent
- Icterus: Absent
- Cyanosis: Absent
- Clubbing: Absent
- Koilonychia: Absent
- Lymphadenopathy: Absent
- Edema: Absent
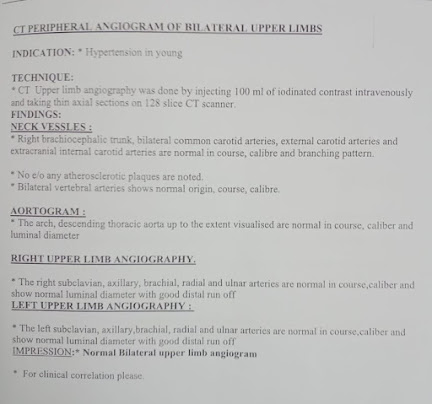
- Right upper limb peripheral pulse feable
- Bi lateral brachial pulses felt
- Bilateral posterior tibial pulses not felt
- Rt UL - 180/100mmHg
- Lt UL - 150/110mmHg
- Rt LL - 190/110mmHg
- Lt LL - 170/100mmHg
SYSTEMIC EXAMINATION:
S1 S2 Heard, no murmurs.
Radio Radial delay and radio femoral delay +
RS: BAE+
ABDOMEN: Soft, non-tender, no organomegaly
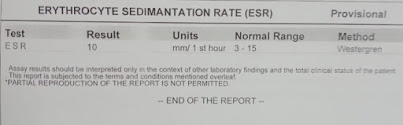
INVESTIGATIONS:
On 22/04/2021
COMPLETE BLOOD PICTURE(CBP)
PROVISIONAL DIAGNOSIS: 34 Year Old Male with Young Onset Hypertension
TREATMENT:
- Tab. CILNIDIPINE 10mg OD
- Tab. CHLORTHALIDONE 12.5mg
- Tab. TELMISARTAN 40mg OD
(DILNIP TRIO)




















Comments
Post a Comment